What is Pancreatic Cancer?
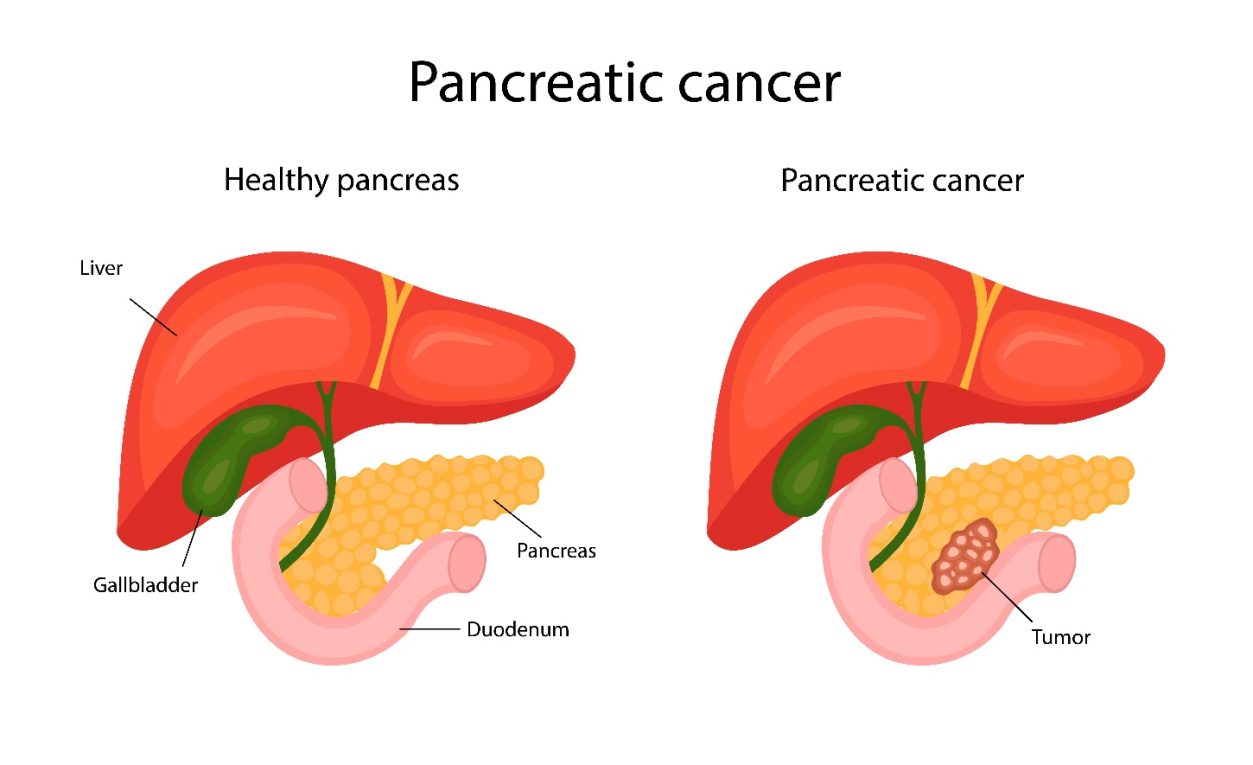
Pancreatic cancer occurs when the cells in the pancreas mutate and become malignant. These abnormal cells grow uncontrollably, form a tumour, and may spread to other parts of the body, making it a life-threatening condition. This type of cancer is often detected late because symptoms may not appear until the tumour has grown significantly or caused pressure in the abdomen.
Patrick Swayze states, “I will go so far as to say probably smoking had something to do with my pancreatic cancer.” (https://www.azquotes.com/quote/647337?ref=pancreatic-cancer).
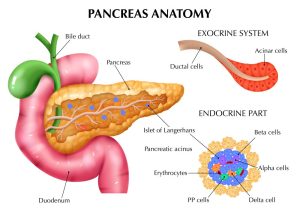
Understanding the Pancreas and Its Functions
The pancreas is a vital organ located behind the stomach and in front of the spine. It has dual functions:
- Endocrine: Produces hormones like insulin to regulate blood sugar.
- Exocrine: Produces digestive enzymes that help break down food.
Types of Pancreatic Cancer
Primary pancreatic cancers are broadly classified into:
1. Exocrine Pancreatic Cancer
- Most common type: Adenocarcinoma, arising from enzyme-producing exocrine cells.
2. Pancreatic Neuroendocrine Tumors (PNETs)
- Originate from hormone-producing endocrine cells.
- These can be benign or malignant and may cause hormonal imbalances.
Pancreatic Cancer Symptoms
Symptoms can be subtle and may mimic other conditions. However, some red flags include:
- Pain in the abdomen or back
- Unexplained weight loss
- Pancreatitis (inflammation of the pancreas)
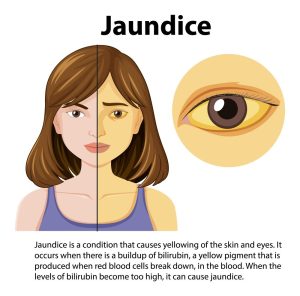
- Jaundice (yellowing of the eyes/skin)
- Dark urine, pale stools, or itching
- Nausea, diarrhea, or loss of appetite
- Fatigue and new-onset type 2 diabetes
- Blood clots (can be an early warning sign)
- Elevated pancreatic polypeptide levels in endocrine tumours.
When to See a Doctor?
Consult your physician if you experience any persistent, unexplained symptoms. Based on initial tests, you may be referred to a gastroenterologist or oncologist to learn more about pancreatic cancer and its treatment.
Pancreatic Cancer Causes
Pancreatic cancer is primarily linked to genetic mutations—either inherited or acquired over time due to environmental exposures. About 10% of cases are considered familial.
Pancreatic Cancer Risk Factors
Factors that may increase your chances of developing pancreatic cancer include:
- Smoking
- Obesity
- Older age
- Chronic pancreatitis
- Family history of pancreatic cancer or related genetic mutations
- Heavy alcohol use
- Liver cirrhosis
- Being male
- Uncontrolled type 2 diabetes

Pancreatic Cancer Prevention
While not entirely preventable, you can reduce risk by:
- Quitting smoking
- Maintaining a healthy weight
- Exercising regularly
- Avoiding excess alcohol
- Controlling diabetes
- Limiting exposure to workplace toxins
- Getting regular health screenings

Pancreatic Cancer Diagnosis
Diagnosing pancreatic cancer can be tricky in its early stages. If cancer is suspected, the following tests may be ordered:
- Blood tests: CA 19-9 levels may be elevated in cancer.
- Ultrasound: Checks for masses or changes in pancreatic structure.
- CT scan: Offers detailed organ imaging, helpful for staging.
- MRI & MRCP/MRA: Show bile and pancreatic duct abnormalities.
- PET scan: Detects metabolic changes in tissues and advanced pancreatic cancer spread.
- Endoluminal Ultrasound (EUS): High-resolution scan via endoscope.
- ERCP: X-ray + endoscopy to assess the bile and pancreatic ducts.
- PTC: X-ray procedure via the liver to assess bile flow blockages.
- Laparoscopy: Minimally invasive surgery to check for metastasis.
- Biopsy: Confirms the cancer diagnosis by examining tissue samples.

Pancreatic Cancer Treatment Options
Treatment depends on the cancer stage, location, type, and the patient’s overall health. Early detection offers a better chance for curative treatment.
-
Surgery
- Whipple Procedure (Pancreatoduodenectomy)
- Distal Pancreatectomy
- Total Pancreatectomy
-
Radiation Therapy
Radiation therapy is used to shrink the tumour before surgery or to control the spread of cancer. Options include
- External Beam Therapy (EBT)
- Stereotactic Body Radiotherapy (SBRT)
- Proton Therapy
-
Chemotherapy
These are cancer drugs administered orally or intravenously to eliminate cancer cells or prevent growth. It may be combined with radiation.
-
Hormonal and Supportive Therapies
In pancreatic neuroendocrine tumors, hormonal disorders may be treated even if the tumour itself is small.
-
Clinical Trials
For patients with advanced pancreatic cancer, clinical trials provide access to innovative therapies and combinations that are still under investigation.

Faqs:
1. What is pancreatic cancer?
Pancreatic cancer is when cancer cells grow in an uncontrolled manner and form masses or tumours in the pancreas. Tumours can impair the pancreas’s ability to function, producing pain and other symptoms.
2. How to prevent pancreatic cancer?
Although it is not possible to completely prevent pancreatic cancer, it is possible to lower the risk by avoiding pancreatic cancer risk factors. On rare occasions, precancerous lesions can be found and removed early to stop the development of pancreatic cancer.
3. What are the pancreatic cancer symptoms?
Early-stage pancreatic cancer does not have any particular symptoms. Still, you should consult your healthcare provider if you experience stomach pain, jaundice (yellowing of the skin), or unintentional weight loss.
4. Can pancreatic cancer patients make a full recovery?
Yes, pancreatic cancer patients can make a full recovery.
5. Is it possible to survive without the pancreas?
It is possible to survive without a pancreas, but you will develop diabetes and need to take insulin regularly. To aid in food digestion, you will also need to take enzyme supplements.
6. What is meant by islet cell cancer?
It is a rare type of pancreatic cancer originating in the cells that make insulin and other hormones.
7. Which doctor treats pancreatic cancer?
An oncologist and gastroenterologist treat pancreatic cancer disease.
References:
https://www.cancer.gov/types/pancreatic/patient/pancreatic-treatment-pdq
https://www.cancer.org/cancer/types/pancreatic-cancer/causes-risks-prevention/prevention.html
https://www.cancer.net/cancer-types/pancreatic-cancer/questions-ask-health-care-team
https://www.cancer.org/cancer/types/pancreatic-cancer/causes-risks-prevention/prevention.html