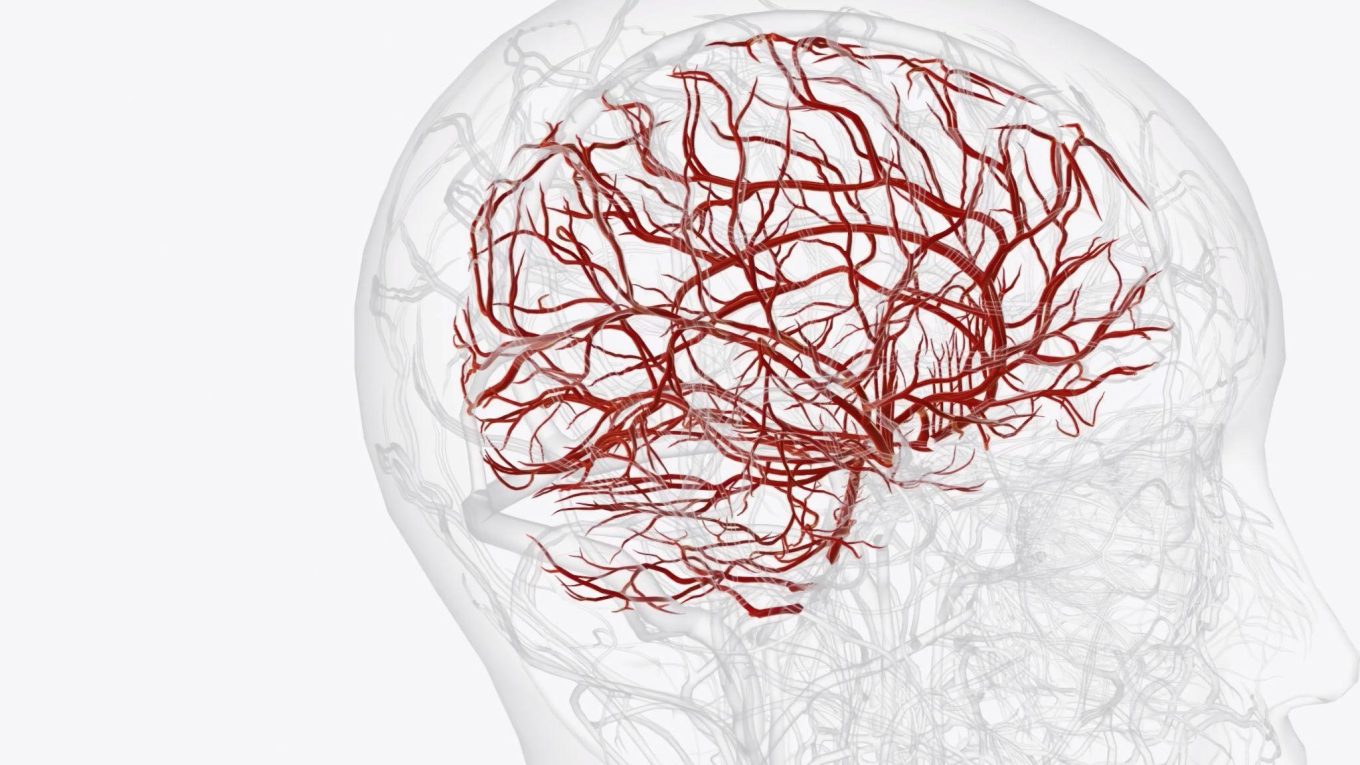
When we think about the brain, we imagine billions of nerve cells working together like a perfectly tuned orchestra, each vessel delivering life-sustaining blood to keep us alive and alert.
But what if, hidden deep inside this orchestra, a few instruments are playing dangerously out of tune? That’s exactly what happens in a condition called Cerebral Arteriovenous Malformation (AVM).
What is AVM?
An Arteriovenous Malformation (AVM) is an abnormal tangle of blood vessels where arteries connect directly to veins without passing through tiny capillaries. In the brain, this abnormality is called a cerebral AVM.
Normally, arteries carry oxygen-rich blood into capillaries, where the exchange of oxygen and nutrients takes place. Veins then carry the oxygen-depleted blood back to the heart. In AVMs, this capillary “bridge” is missing, causing blood to rush directly from arteries to veins causing high pressure on veins, making them prone to rupture and bleeding.
AVMs can develop anywhere in the body, but cerebral AVMs are the most dangerous because they affect brain tissue, potentially leading to seizures, strokes, or permanent neurological damage.
Causes of Cerebral AVM
The exact cause of AVM formation is not completely understood. However, research suggests:
- Congenital factors – Most cerebral AVMs are thought to develop before birth. Abnormal vessel development during fetal growth may trigger this condition.
- Genetic influences – Though most AVMs are not inherited, certain genetic syndromes such as Hereditary Hemorrhagic Telangiectasia (HHT) may increase the likelihood.
- Developmental irregularities – Some AVMs may form later in life due to abnormal blood vessel remodeling.
AVMs are structural abnormalities that arise during early development and are not influenced by lifestyle choices such as diet, smoking, or exercise.
Arteriovenous Malformation Symptoms
Symptoms vary widely depending on the size and location of the AVM. Some people remain asymptomatic and discover the malformation accidentally during brain scans for unrelated reasons. However, many present with noticeable arteriovenous malformation symptoms such as:
- Headaches – Often persistent and sometimes resembling migraines.
- Seizures – Sudden abnormal electrical activity due to disrupted brain blood flow.
- Vision problems – Blurred or double vision, especially if AVM is near the optic nerve.
- Weakness or numbness – On one side of the body.
- Difficulty speaking or understanding – If AVM affects language centers.
- Unexplained dizziness or balance issues.
When bleeding occurs, symptoms escalate dramatically:
- Sudden severe headache (often described as the worst headache ever experienced).
- Nausea, vomiting, and loss of consciousness.
- Sudden weakness, paralysis, or seizures.
These emergencies require immediate medical attention, as ruptured AVMs can cause life-threatening brain hemorrhage.
AVM Brain Symptoms
Because cerebral AVMs directly affect brain tissue, the neurological signs are often localized. For instance:
- AVMs in the frontal lobe may cause behavioral changes, difficulty concentrating, or motor weakness.
- In the temporal lobe, patients may experience memory disturbances or seizures.
- In the occipital lobe, vision problems are common.
- Deep brain AVMs may cause subtle but progressive issues with movement, coordination, and sensation.
Thus, AVM brain symptoms often mimic stroke or brain tumor presentations, making an accurate diagnosis essential.
Diagnosing Cerebral AVM: Role of Radiology
Common cerebral AVM radiology tools include:
- MRI (Magnetic Resonance Imaging) – Provides detailed brain images to show the exact location and size of the AVM.
- CT Scan – Helps detect bleeding and structural abnormalities.
- Cerebral Angiography (DSA – Digital Subtraction Angiography) – The gold standard test where contrast dye is injected into brain vessels to visualize the AVM structure and blood flow.
- MRA (Magnetic Resonance Angiography) and CTA (CT Angiography) – Less invasive ways to map the abnormal vessels.
Risks Associated with Cerebral AVM
The most concerning risks include:
- Brain Hemorrhage (Bleeding) – Rupture of fragile vessels is the most dangerous complication, with a mortality risk of up to 10% during the first bleed.
- Seizures – Chronic abnormal electrical activity due to disrupted brain perfusion.
- Stroke-like symptoms – Weakness, numbness, or speech difficulties due to reduced blood supply.
- Progressive neurological damage – Even without rupture, AVMs may compress nearby brain tissue and impair function.
- Cognitive and psychological effects – Memory loss, concentration issues, anxiety, and depression may result.
AVM Treatment Options
Major avm treatments are:
1. Surgical Resection
- Suitable for AVMs located in accessible brain regions.
- The surgeon removes the entire AVM, eliminating the risk of future bleeding.
- Carries risks of infection, stroke, or neurological deficits.
2. Endovascular Embolization
- A minimally invasive procedure where a catheter is threaded through blood vessels, and glue-like material is injected to block abnormal connections.
- Often performed as a standalone therapy or before surgery/radiosurgery to shrink the AVM.
3. Stereotactic Radiosurgery (Gamma Knife or CyberKnife)
- Uses targeted radiation beams to damage AVM vessels, causing them to close over time.
- Best for small to medium AVMs.
- Takes months to years for full effect, but less invasive compared to open surgery.
4. Combined/Multimodal Therapy
- In many cases, doctors combine embolization, radiosurgery, and microsurgery for best results.
5. Medical Management
- If treatment risks outweigh benefits, patients may be managed with seizure medications, regular imaging, and lifestyle adjustments while monitoring closely.
Conclusion:
Cerebral Arteriovenous Malformations may be rare, but their potential risks demand attention. Understanding what an AVM is, recognizing its symptoms early, and seeking advanced imaging through cerebral AVM radiology are critical steps in diagnosis. With modern AVM treatment options ranging from surgery to radiosurgery, patients now have better outcomes than ever before.