A comprehensive guide to understanding Triple Negative Breast Cancer: from diagnosis to cutting-edge treatments
Understanding Triple Negative Breast Cancer: The Basics
Triple Negative Breast Cancer (TNBC) represents one of the most challenging forms of breast cancer to treat, yet recent advances in medical research are bringing new hope to patients and their families. Triple-negative breast cancer (TNBC) accounts for about 10-15% of all breast cancers, making it a significant concern in oncology practice.
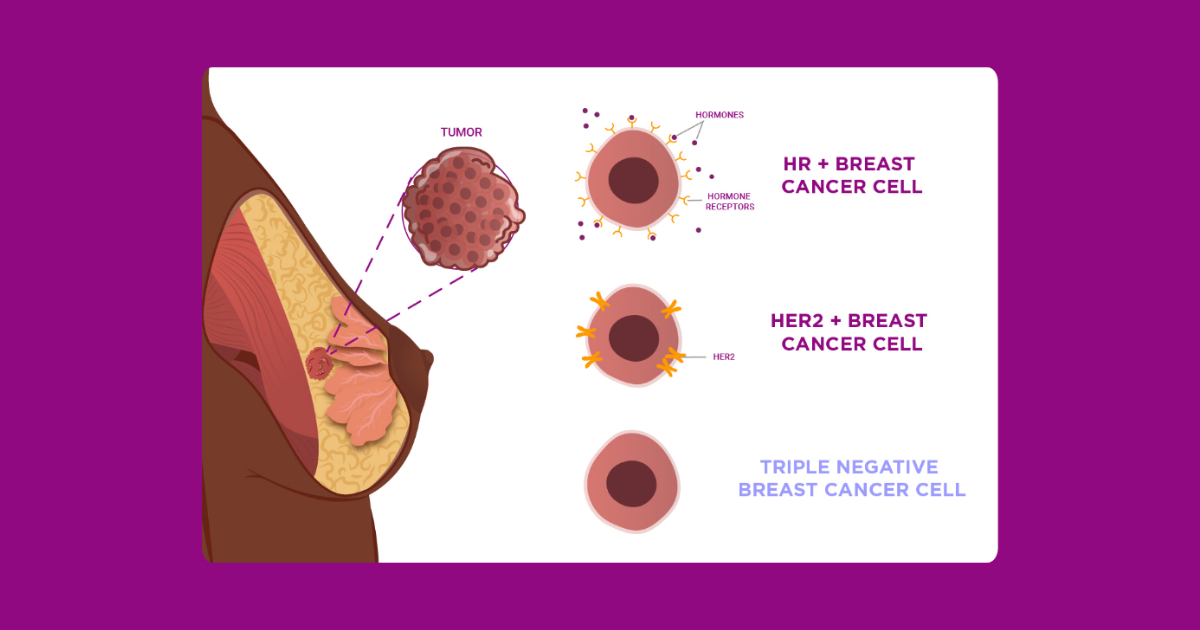
Triple-negative breast cancer is an aggressive type of breast cancer that can be hard to treat and often comes back. The term “triple negative” refers to the absence of three specific receptors that are commonly found in other breast cancers:
- Estrogen Receptor (ER): Negative
- Progesterone Receptor (PR): Negative
- Human Epidermal Growth Factor Receptor 2 (HER2): Negative
This unique characteristic makes TNBC distinct from other breast cancer subtypes and significantly impacts treatment approaches, as many standard hormonal therapies and targeted treatments are ineffective against this form of cancer.
The Current Landscape: Statistics and Trends
Prevalence and Demographics
The statistics surrounding TNBC reveal important patterns that help us understand who is most at risk:
Triple-negative breast cancer accounts for approximately 15% to 25% of all breast cancers. Based on data from 2021, in the United States (US) the overall age-adjusted incidence of triple-negative breast cancer is 14.5 cases per 100,000 women.
Racial and Ethnic Disparities:
Non-Hispanic Black women are most likely to be diagnosed with TNBC compared to other racial groups. 1 in 5 Black women with breast cancer are diagnosed with triple-negative breast cancer, which is harder to treat. This is higher than any other racial or ethnic group.
Age Factors:
Premenopausal women and women under the age of 50 have an increased risk of developing TNBC. This younger age of onset is one of the distinguishing characteristics that sets TNBC apart from other breast cancer types.
Survival Rates: Understanding the Numbers
The survival statistics for TNBC vary significantly depending on the stage at diagnosis:
Early-Stage TNBC: Although research suggests that about 40% of people who receive treatment for stages 1 to 3 of TNBC will experience a recurrence, 60% will continue to live a disease-free survival.
Advanced TNBC: Metastatic triple-negative breast cancer is an aggressive cancer with an average survival of 8 to 13 months, though survival for patients newly diagnosed with metastatic (stage IV) triple-negative breast cancer is about 1 ½ to 2 years with current treatments.
Five-Year Survival: In the United States, TNBC is responsible for 12% of breast cancers, with a 5-years survival rate of 8–16% for metastatic disease, though early-stage survival rates are significantly better.
Recognizing the Symptoms: What to Watch For
TNBC often presents with symptoms similar to other breast cancers, but Triple-negative breast cancer is a fast-growing form of breast cancer, which means symptoms may develop more rapidly than with other types.
Common Symptoms Include:
Physical Changes:
- A new lump or mass in the breast or underarm area
- Changes in breast size or shape
- Skin dimpling or puckering
- Nipple inversion or discharge
- Redness, scaliness, or thickening of breast skin
Advanced Symptoms:
- Bone pain (if cancer has spread to bones)
- Shortness of breath or persistent cough (lung involvement)
- Abdominal swelling or loss of appetite (liver involvement)
- Severe headaches or vision changes (brain involvement)
Why Early Detection Matters
Due to the aggressive nature of TNBC, early detection is crucial. Triple-negative breast cancer (TNBC) represents a particularly aggressive and heterogeneous subtype of breast cancer, associated with poor prognosis and limited treatment options. However, when caught early, treatment outcomes improve significantly.
Understanding Risk Factors: Who’s at Higher Risk?
Genetic Predisposition
The connection between genetic mutations and TNBC is one of the most significant risk factors:
BRCA Mutations: We’ve known that mutations in the BRCA1 and BRCA2 genes are linked with an increased risk for breast cancer. Now we know 5 other genes associated with a high risk for triple-negative breast cancer (TNBC).
Some women with triple negative breast cancer also have a fault (mutation) in the BRCA1 or BRCA2 genes. BRCA stands for Breast Cancer gene. Everyone has BRCA1 and BRCA2 genes. They stop cells in our body from growing and dividing out of control.
Implications for Families: Women with BRCA1 mutations have a significantly higher lifetime risk of developing TNBC. CBC incidence at 60, 120, and 150 months was significantly higher in BRCA1/2 mutation carriers compared to non-carriers.
Age and Hormonal Factors
Age Distribution: The risk is 4.2% among women aged less than 40 years. It was also noted that when the duration of oral contraceptive use increased, the risk increased.
Additional Risk Factors
Lifestyle and Environmental:
- History of radiation therapy to the chest
- Dense breast tissue
- Personal or family history of breast or ovarian cancer
- Certain benign breast conditions
Reproductive History:
- Early menstruation (before age 12)
- Late menopause (after age 55)
- Never having been pregnant or having first pregnancy after age 30
Modern Treatment Approaches: Hope Through Innovation
Traditional Chemotherapy: The Foundation
Out of these, chemotherapy is the most established treatment for TNBC. Unlike hormone receptor-positive breast cancers that can be treated with hormonal therapies, TNBC requires more aggressive approaches.
Neoadjuvant Chemotherapy:
- Given before surgery to shrink tumors
- Allows for breast-conserving surgery in some cases
- Provides insight into how well the cancer responds to treatment
Adjuvant Chemotherapy:
- Given after surgery to eliminate remaining cancer cells
- Reduces risk of recurrence
- Typically includes combinations of drugs like anthracyclines and taxanes
Revolutionary Immunotherapy
If TNBC comes back (recurs) locally, cannot be removed with surgery, and makes the PD-L1 protein, immunotherapy with the drug pembrolizumab along with chemotherapy is an option.
Key Immunotherapy Advances: immune checkpoint inhibitors, for example, pembrolizumab, atezolizumab, and durvalumab, are widely explored for TNBC treatment.
Recent studies show promising results: A promising clinical trial shows that a combination of paxalisib, pembrolizumab, and chemotherapy significantly reduces circulating tumor cells in metastatic triple-negative breast cancer.
Targeted Therapy Breakthroughs
PARP Inhibitors: Targeted therapies, including PARP inhibitors, immune checkpoint inhibitors, and EGFR inhibitors, hold promise for personalized treatment approaches. These drugs are particularly effective in patients with BRCA mutations.
Antibody-Drug Conjugates (ADCs): Sacituzumab govitecan is the next game-changer for treating metastatic triple-negative breast cancer with 2X longer survival rates than the single-agent chemotherapies.
Other Targeted Approaches: These include PI3K/AKT/mTOR inhibitors, epidermal growth factor receptor inhibitors, Notch inhibitors, poly ADP-ribose polymerase inhibitors, and antibody–drug conjugates.
Combination Therapies: The Future of Treatment
The therapeutic strategies include immunotherapy and various molecular targeted therapies, including intracellular pathway inhibitors, cell cycle inhibitors, and AR inhibitors.
Multi-Modal Approaches: interventions have been highlighted and include chemotherapy, immunotherapy, radiotherapy, stem cell therapy, laser treatment, hyperthermia, surgery, and photodynamic therapy.
The Treatment Journey: What Patients Can Expect 
Diagnosis and Staging
Initial Evaluation:
- Comprehensive physical examination
- Imaging studies (mammography, ultrasound, MRI)
- Biopsy for definitive diagnosis
- Staging studies to determine extent of disease
Molecular Testing:
- Confirmation of triple-negative status
- BRCA and other genetic testing
- PD-L1 expression testing for immunotherapy eligibility
Treatment Planning
Multidisciplinary Team Approach:
- Medical oncologist
- Surgical oncologist
- Radiation oncologist
- Genetic counselor
- Nursing specialists
- Social workers and patient navigators
Surgery Options
Breast-Conserving Surgery:
- Lumpectomy with radiation therapy
- Suitable when tumor size allows
- Preserves breast appearance
Mastectomy:
- Complete breast removal
- May be recommended for larger tumors
- Reconstruction options available
Recovery and Follow-Up
Short-term Recovery:
- Managing treatment side effects
- Regular monitoring during active treatment
- Support services for physical and emotional well-being
Long-term Surveillance:
- Regular follow-up appointments
- Imaging studies as recommended
- Monitoring for signs of recurrence
Prevention and Risk Reduction
For High-Risk Individuals
Surveillance Strategies:
- Enhanced screening protocols
- MRI in addition to mammography
- Clinical breast examinations
- Self-examination education
Risk Reduction Options:
- Prophylactic surgery consideration
- Lifestyle modifications
- Chemoprevention discussions
- Regular genetic counseling updates
Looking Forward: The Future of TNBC Treatment
Emerging Technologies
Precision Medicine:
- Tumor profiling for personalized treatment
- Liquid biopsy for monitoring
- Artificial intelligence in diagnosis
- Genomic testing advancements
Novel Therapeutic Approaches:
- CAR-T cell therapy development
- Novel drug delivery systems
- Combination immunotherapy strategies
- Resistance prevention protocols
Hope Through Research
Triple-negative breast cancer (TNBC) was first described as a distinct disease entity 20 years ago. Since that time, there has been tremendous effort invested in understanding the clinical features and biology of this breast cancer subtype and developing effective treatments.
Despite the challenges, Despite the approval of new TNBC targeted therapies, only a month increase of the 5-year survival rate was observed, researchers continue to make significant strides in understanding and treating this complex disease.
Key Takeaways for Patients and Families
- Early Detection Saves Lives: Regular screening and awareness of symptoms are crucial, especially for high-risk individuals.
- Treatment is Evolving: New therapies are continually being developed and approved, offering improved outcomes.
- Genetic Testing Matters: Understanding your genetic risk can guide treatment decisions and family planning.
- Support is Available: Comprehensive support services can significantly improve quality of life during treatment.
- Hope is Justified: While TNBC is aggressive, many patients achieve excellent outcomes with current treatments.
- Research Participation: Clinical trials offer access to cutting-edge treatments and contribute to advancing care for all patients.