COLORECTAL CANCER
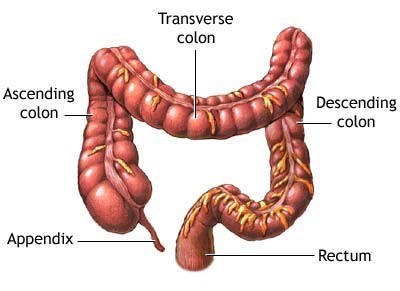
A cancer of the colon or rectum, located at the digestive tract's lower end. The colon and rectum make up the large intestine (or large bowel), which is part of the digestive system.
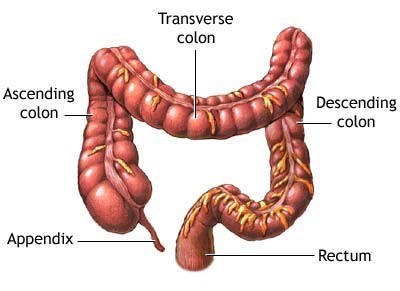
- The first section is called the ascending colon. It starts with a pouch called the cecum, where undigested food is comes in from the small intestine. It continues upward on the right side of the abdomen (belly).
- The second section is called the transverse colon. It goes across the body from the right to the left side.
- The third section is called the descending colon because it descends (travels down) on the left side.
- The fourth section is called the sigmoid colon because of its “S” shape. The sigmoid colon joins the rectum, which then connects to the anus.
 Risk Factors
Risk factors you can change:
Risk Factors
Risk factors you can change:
- Being overweight or obese
- Certain types of diets - A diet that's high in red meats (such as beef, pork, lamb, or liver) and processed meats raises your colorectal cancer risk.
- Smoking
- Alcohol use
Risk factors you cannot change:
- Being older: Your risk of colorectal cancer goes up as you age. Younger adults can get it, but it's much more common after age 50.
- History of colorectal polyps or colorectal cancer: with a history of adenomatous polyps you are at increased risk of developing colorectal cancer. This is especially true if the polyps are large, if there are many of them, or if any of them show dysplasia. If you've had colorectal cancer, even though it was completely removed, you are more likely to develop new cancers in other parts of the colon and rectum. The chances of this happening are greater if you had your first colorectal cancer when you were younger.
- Lynch syndrome (hereditary non-polyposis colon cancer or HNPCC): Lynch syndrome is the most common hereditary colorectal cancer syndrome. It accounts for about 2% to 4% of all colorectal cancers. The cancers linked to this syndrome tend to develop when people are relatively young. People with Lynch syndrome can have polyps, but they tend to only have a few. The lifetime risk of colorectal cancer in people with this condition may be as high as 50% , but this depends on which gene is affected. Other cancers linked with Lynch syndrome include cancer of the endometrium, ovary, stomach, small intestine, pancreas, kidney, prostate, breast, ureters and bile duct.
Staging:
The most often used for colorectal cancer is the TNM system, which is based on 3 key pieces of information:
-
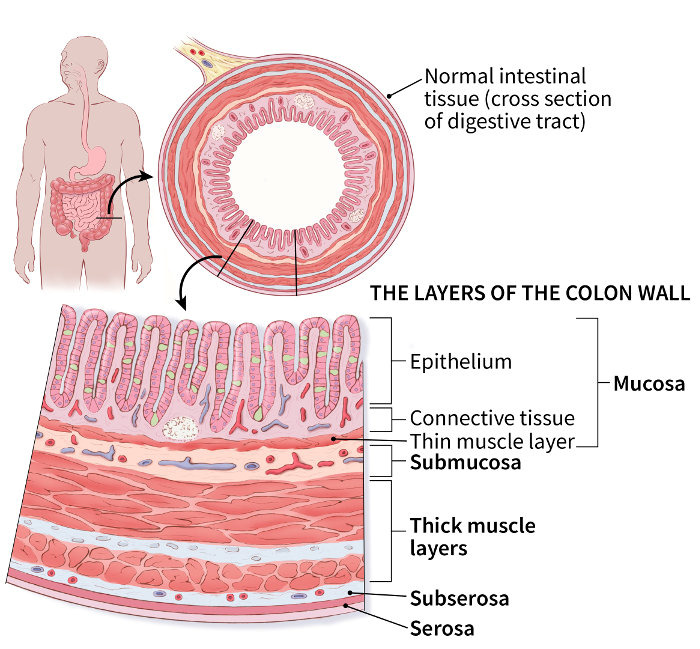
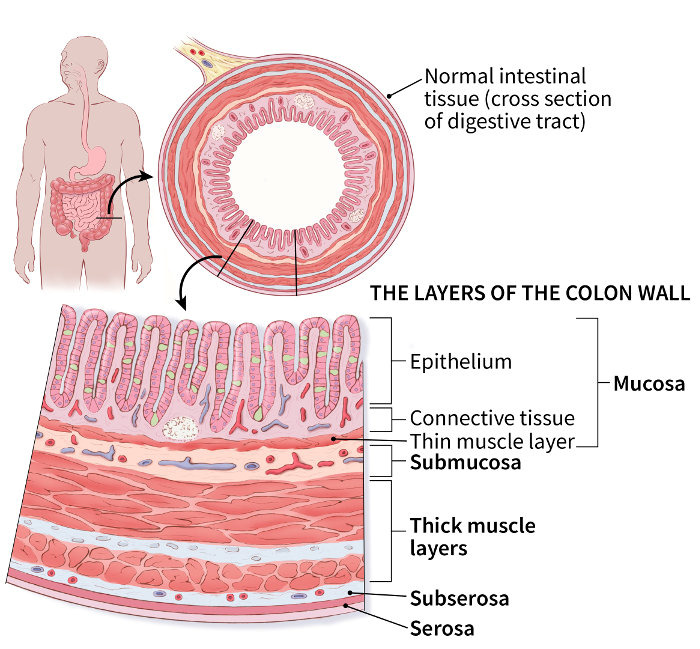
The extent (size) of the tumor (T): How far has the cancer grown into the wall of the colon or rectum? These layers, from the inner to the outer, include:
- The inner lining (mucosa), which is the layer in which nearly all colorectal cancers start. This includes a thin muscle layer (muscularis mucosa).
- The fibrous tissue beneath this muscle layer (submucosa)
- A thick muscle layer (muscularis propria)
- The thin, outermost layers of connective tissue (subserosa and serosa) that cover most of the colon but not the rectum.
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs such as the liver or lungs?
Treatment
Surgery
The primary treatment for colorectal cancer is often surgical removal of the cancerous part and surrounding lymph nodes, along with a length of normal tissue on either side of the cancer.
Many of these surgeries can be done using a minimally invasive or robotic approaches.
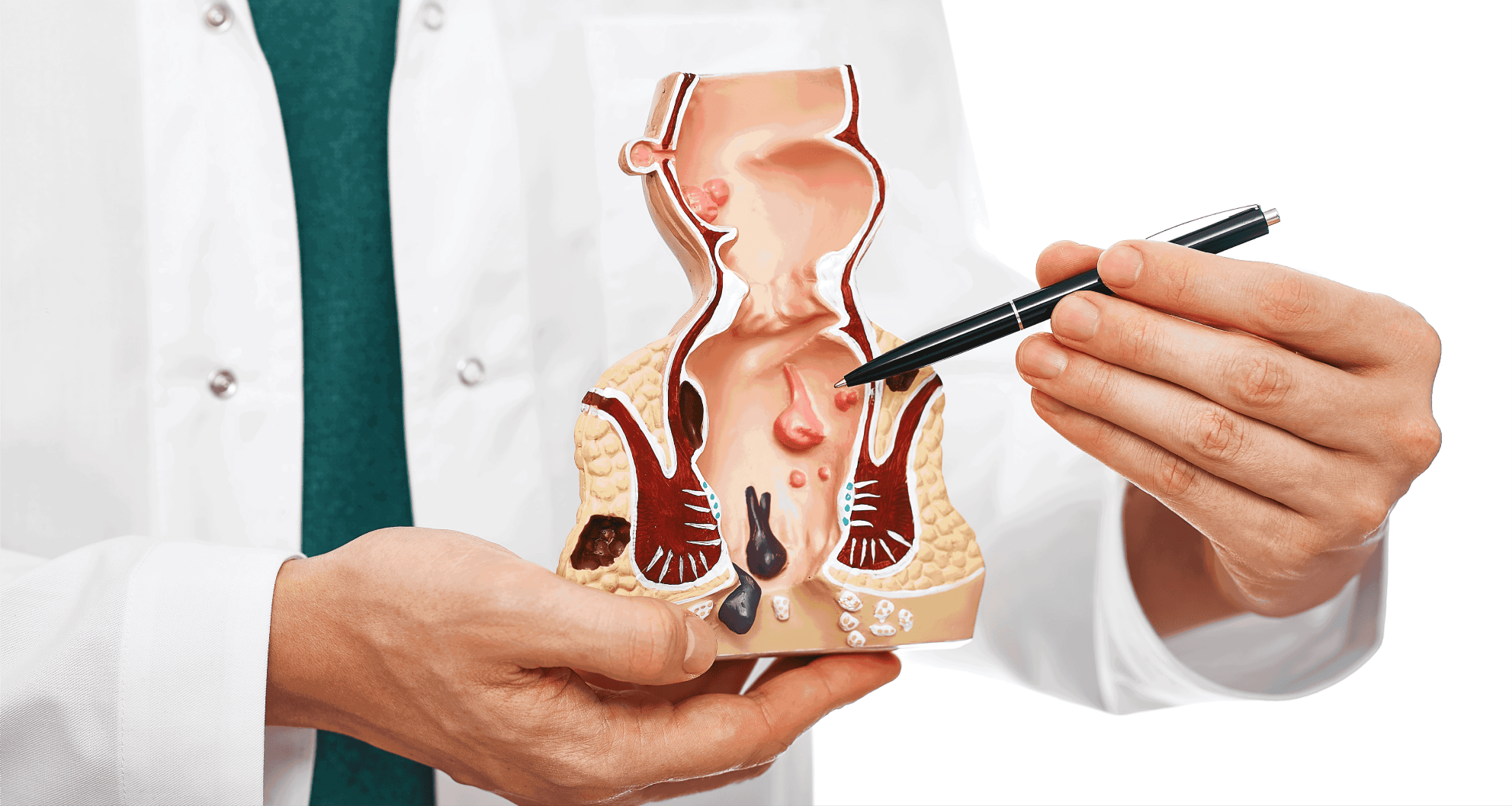
- Removing polyps during a colonoscopy (polypectomy): If your cancer is small, localized, completely contained within a polyp and in a very early stage, your doctor may be able to remove it completely during a colonoscopy.
- Endoscopic mucosal resection. Larger polyps might be removed during colonoscopy using special tools to remove the polyp and a small amount of the inner lining of the colon in a procedure called an endoscopic mucosal resection.
- Minimally invasive surgery (laparoscopic surgery). Polyps that can't be removed during a colonoscopy may be removed using laparoscopic surgery. Surgery is performed through several small incisions in your abdominal wall, inserting instruments with attached cameras that display your colon on a video monitor. The surgeon may also take samples from lymph nodes in the area where the cancer is located.
- Partial colectomy. the surgery involves removal of the part of the colon that contains the cancer, along with a margin of normal tissue on either side of the cancer. most often its is possible to reconnect the healthy portions of your colon or rectum.
- Surgery to create a way for waste to leave your body. If its not possible to reconnect the healthy portions of your colon or rectum, you may need an ostomy. This involves creating an opening in the wall of your abdomen from a portion of the remaining bowel for the elimination of stool into a bag that fits securely over the opening.
Sometimes the ostomy is only temporary, allowing your colon or rectum time to heal after surgery. In some cases, however, the colostomy may be permanent.
- Lymph node removal. Nearby lymph nodes are usually also removed during colon cancer surgery and tested for cancer.
Palliative resections are recommend If cancer is very advanced or your or to relieve a blockage of your colon or in order to improve your symptoms. This surgery isn't done to cure cancer, but instead to relieve signs and symptoms, such as a blockage, bleeding or pain.
Medical Therapy
Chemotherapy to destroy cancer cells using strong anti-cancer drugs
- Chemotherapy: Chemotherapy eliminates cancer cells that are growing. Chemotherapy may be used to control disease that cannot be operated on, get rid of cancer cells after surgery or shrink cancer before a surgery.
- Immunotherapy: Medications that alter your immune system’s response to cancer may be appropriate therapy in some cases of colon and rectal cancer, specifically cancers associated with Lynch syndrome.
- Molecular therapy: Medications that target specific mutations in your cancer may be recommended in addition to chemotherapy. Your tumor will be evaluated for any mutations that can be targeted with molecular therapy.
Radiation Therapy
It is delivered using a radiation beam from a linear accelerator (linac) directed at the tumor with computed tomography (CT) or magnetic resonance imaging (MRI) guidance. The CT or MRI guidance allows the most radiation to be directed at the tumor while minimizing how much radiation your normal, healthy tissues get.
Radiation treatment options include:
AI BASED RADIOTHERAPY: This therapy can be a more precise treatment that limits the radiation exposure of normal tissues around the targeted tumor. This can be helpful in certain locations in the body and with certain types of cancers. Omega hospitals is the first and only health system in the country to offer AI Based Radiotherapy.
- Three-dimensional conformal radiation therapy (3D-CRT): Detailed 3D images are created using CT or MRI scans to direct the radiation beam to the tumor and any surrounding tissue that may be affected by cancer.
- Intensity modulated radiation therapy (IMRT): High-precision radiotherapy delivers different radiation doses to different parts of the tumor.
- Stereotactic radiotherapy (SBRT): This radiation procedure delivers a single high-dose radiation treatment to a cancerous tumor. This may be appropriate for smaller tumors.
Targeted Therapies
- Radioembolization: Interventional radiologists block a tumor's blood supply with radioactive isotopes. This also delivers radiation with more precision and spares healthy tissue from unnecessary radiation. This minimally invasive procedure may be used if your colorectal cancer has spread to the liver.
- Chemoembolization: A specially trained interventional radiologist can provide anti-cancer medications directly into a tumor through the blood supply it depends on. This allows a higher concentration of the medication to have longer contact with the tumor.
Palliative Medicine
Side effects from cancer treatment can affect your quality of life and how your body responds to treatment.
- Treat pain and other physical symptoms of cancer, such as fatigue, nausea, trouble sleeping, poor appetite, breathing problems and weight loss.
- Treat any emotional symptoms, such as depression and anxiety.
- Improve your body’s ability to tolerate cancer treatments.
 Risk Factors
Risk factors you can change:
Risk Factors
Risk factors you can change: